
Fungal Nail/ Onychomycosis
Onychomycosis is an infection of the nail plate and/or nail bed caused by fungi, which are microscopic plant-based organisms that do not contain chlorophyll and as such are unable to photosynthesise so instead rely on organic matter for food.
The most common fungi involved in Onychomycosis are classified as dermatophytes, these organisms have the ability to metabolise keratin allowing them to thrive.
Most commonly the infection begins at the tip of the nail usually in a corner (Distal Subungual Onychomycosis) and slowly spreads towards the lunula (the white crescent part of the nail) discolouring the nail which may become brittles and crumble away. As this occurs the build up of debris beneath the nail plate can cause it to lift and separate from the nail bed.
Multiple factors can increase your chance of a fungal nail infection, the chief among them being.
- Restrictive, non-breathable footwear
- Hyperhidrosis/ Excessively sweating feet
- Improper drying of the feet
- Progression of an existing condition such as Athletes foot/ Tinea Pedis
- Damage to the nail plate
- Regular exposure to communal areas such as shower rooms, swimming pools, gyms
To help minimise the risk of infection it is recommended.
- Treat Athletes foot as soon as possible
- Wear flipflops in communal changing areas and shower rooms
- Ensure to dry your feet thoroughly after bathing, taking care to dry between your toes
- Wear cotton socks, avoiding synthetic materials which can cause your feet to sweat further.
- Wear fresh socks daily
- DO NOT share towels
- Wear breathable shoes
- Avoid painting infected nails as this can trap moisture
Treatment options
With average nail growth being approximately 1.6mm per month it can take a very long time to resolve Onychomycosis between 12-16+ months with more advanced cases requiring oral medications prescribed by your GP.
With such a long a treatment time it is paramount to begin treating suspected fungal nail as soon as practicably possible and maintain treatment until the infection has cleared.
There is a wide range of antifungals available both over the counter and prescribed, depending on your individual needs.
For mild cases presenting within the clinic, treatment includes through debriding, thinning and trimming back of the infected nails with the following advice for ongoing care.
- Scholl fungal nail treatment kit: File the nail surface once weekly disposing of the file after use and applying the nail lacquer daily until the infection has grown out.
- Scholl Athletes foot spray: spray the insides of footwear and allow to dry thoroughly before wearing. Apply to areas of Athletes foot twice daily again allowing to dry before wearing socks or footwear.
- Milton’s sterilising tablets: We recommend washing socks and hosiery with a sterilising tablet at the beginning of your treatment to help minimise reinfection.
What causes warts and verrucas
What causes warts and how to minimise the risk of spreading them.
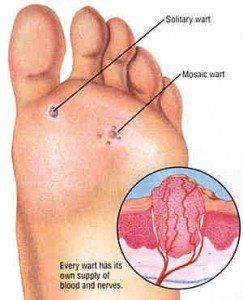
Warts and verrucae are caused by the human papilloma virus (HPV). There are over 150 different types of HPV but most warts are caused by only a few specific types. The virus infects cells in your skin, causing it to thicken and coarsen.
Warts and verrucae can spread from person to person by direct skin contact. They can also spread by contact with floors or surfaces contaminated with the virus. Although warts are contagious, it’s thought that the risk of catching them is fairly low. You’re more likely to get infected if your skin is damaged or wet, so infection can be linked to swimming pools and communal showers. You can also infect yourself. If you scratch a wart or verruca, the viral particles may spread to other areas of your skin.
You’re more likely to develop warts and verrucae if you have a weakened immune system, for example because you have had an organ or stem cell transplant.
Prevention of warts and verrucae
Warts and verrucae are usually caused by direct skin contact or contact with surfaces contaminated with the human papilloma virus (HPV).
It’s hard to completely avoid coming into contact with HPV. Taking the following precautions may help to prevent warts and verrucae.
• Try not to touch other people’s warts or verrucae.
• Don't share your towels, shoes or socks.
• Wear flip-flops in communal showers.
• Cover your wart or verruca with a waterproof plaster when you go swimming.
• Don't scratch or pick your wart or verruca as it’s more likely to spread.
• If you use nail files or pumice stones on your wart or verruca, don’t use these on other areas of your skin.
Remember – there’s no reason why you can’t continue to take part in activities, such as sports or swimming, if you have a wart or verruca. But do follow all the advice above, to avoid passing the virus onto other people.

Ingrown Toenails
Onychocryptosis is a common condition with approximately 10,000 reported cases each year in the UK. In most cases ingrown toenails occur gradually due to continual pressure on the nail or a nail spur left during improper trimming, growing towards the free edge.
As the nail grows out the sharp spur slowly digs into and eventually pierces the surrounding tissue causing swelling and pain. This inflammatory response is easily characterised as the area will be swollen, tender and warm to the touch with a reddened appearance.
multiple factors can contribute to ingrown nails the most common being.
- Improperly fitting and excessively pointed footwear
- Improper cutting of toenails, leaving sharp edges
- Trauma to the toe
Predominantly ingrown nails affect the Hallux (big toe) but can affect the lower digits as well, treating this condition as soon as practicably possible can save a lot of discomfort and the need for surgical intervention.
Minor to mild cases can be treated by a Footcare practitioner with slightly varying methods employed depending on individual circumstances including.
- Drainage of infection site
- Application of both topical antiseptics and Inadine gauze
- Removal of nail fragments or spurs and filling the nail edge smooth again.
- Gentle lifting of the lateral edge of the nail and insertion of Inadine gauze and Tapenade to allow the nail to grow out.
- Tubular dressing for the digit in question.
A check up appointment is then required to monitor infection and replace the dressing, gauze and tapenade.
In severe cases where the nail has penetrated deep into the surrounding tissues and serious infection has occurred referral to an NHS podiatrist is required, where antibiotics may be prescribed to clear the infection before the offending nail is surgically removed, at this point the nail bed and matrix may also be treated to prevent nail regrowth.
